Unlock The Door to Medical Billing Success With our Comprehensive Credentialing Services
Our steadfast dedication to excellence empowers you to prioritize what truly matters. As a leading medical billing company, we relentlessly pursue excellence and are fully committed to providing exceptional coding services to healthcare providers worldwide.
Request a Demo
Comprehensive Medical Billing
Services to Optimize Your
Revenue Cycle
At EHS, we understand that medical billing is a critical component of your healthcare practice. That is why we offer comprehensive medical billing services to help you manage your revenue cycle effectively and maximize your revenue. Our team of experienced billing experts has the knowledge and expertise to handle all aspects of medical billing, from claims submission to denial management.
Our medical billing services are designed to be flexible and customizable, to meet the unique needs of your healthcare practice. Whether you are a solo practitioner or a large healthcare organization, we have the expertise and resources to help you manage your revenue cycle effectively.
Types of Credentialing
There are different types of credentialing that healthcare providers and facilities may need to complete, including:
Provider Credentialing
The process of verifying the qualifications of individual healthcare providers, such as physicians, nurses, and therapists.
Facility Credentialing
The process of verifying the qualifications of healthcare facilities, such as hospitals, clinics, and ambulatory surgery centers.
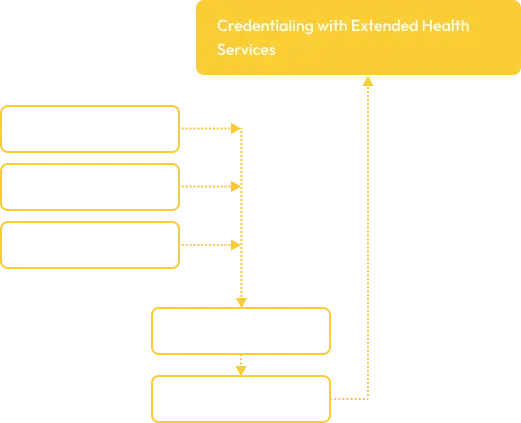
Credentialing Process with EHS Medical
Billing Credentialing
At EHS Medical Billing Services, we understand that the credentialing process can be time-consuming and complex. That is why we offer comprehensive credentialing services to healthcare providers and facilities. Our credentialing specialists can assist you with every step of the process, including:
1
Collecting and completing the necessary paperwork and applications
2
Verifying your credentials with insurance companies and other third-party payers
3
Following up with payers to ensure that the credentialing process is completed in a timely manner
Importance of Credentialing in Medical
Billing Efficiency
Credentialing is an essential step in the medical billing process, as it ensures that healthcare providers and facilities are qualified to provide healthcare services. By completing the credentialing process, you can:
1. Increase your revenue by participating in medical billing
2. Increase your revenue by participating in medical billing
3. Increase your revenue by participating in medical billing
Common Challenges in the Credentialing
Process
At EHS Medical Billing Services, our experienced credentialing specialists can help you overcome these challenges and ensure that the credentialing process is completed in a timely and efficient manner.
The credentialing process can be complex and time-consuming, and there are several common challenges that healthcare providers and facilities may face, such as:
1. Missing or incomplete paperwork
2. Delays in the credentialing process
3. Lack of knowledge about the credentialing process
Unlock Your Medical Billing Potential with Our
Comprehensive Credentialing Services
At EHS Medical Billing Services, we understand the importance of credentialing in the medical billing process. That is why we offer comprehensive credentialing services to healthcare providers and facilities. By completing the credentialing process, you can increase your revenue, establish credibility, and improve patient outcomes. Contact us today to learn more about our credentialing services.
Frequently Asked Questions about Extended Health Services
Everything you need to know about the Extended Health Services.
